Pathogen of the Month - 2018 Archive
December pathogen of the month:
Ebola
What is it? Ebola is a deadly viral disease that affects primates – including people, monkeys, gorillas and chimpanzees. It is caused by any of four varieties of the ebolavirus.
It is endemic in Africa, mostly within the Congolese forest basin.
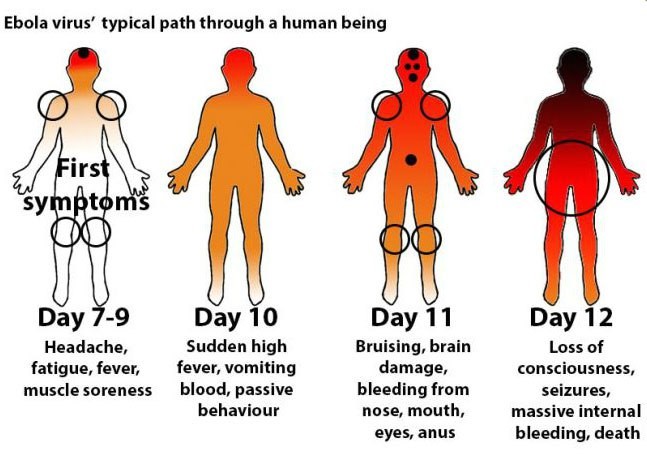
Symptoms include fever, headache, muscle pain, weakness, fatigue, diarrhea, vomiting and abdominal pain. Those symptoms may appear any time from two to 21 days following contact with the virus and often evolve toward a severe hemorrhagic syndrome, and death in half the cases.
Scientists hypothesize that bats are the reservoir host for the virus in the tropical rainforests of Africa, and that they transmit it to other animals, commonly apes but also occasionally antelopes. Humans can also acquire the virus by direct contact with infected bats or other infected animals.
History: The Centers For Disease Control says Ebola virus was discovered in 1976 near the Ebola River in what is now the Democratic Republic of Congo (DRC) in central Africa.
Since then there have been 21 outbreaks, including an ongoing outbreak that began this past May in the DRC. Scientists now believe the virus long pre-dated the first known outbreak, with risk factors such as population growth, encroachment into forested areas and direct interaction with wildlife contributing to its occurrence and spread within human populations.
The 2014 outbreak is probably the best known because it transcended the boundaries of tropical Africa, reaching as far as Italy, Spain and the United States. In the U.S., four imported cases were reported with one fatality. Most of the infected parties acquired the virus during overseas travel in tropical Africa. No secondary cases were reported in the U.S.
|
Map of ebola outbreaks by species and size since 1976 |
Mode of transmission. Ebola is most commonly spread to people via direct contact with the bodily fluids of a sick person. It can also be spread through direct contact with the blood, bodily fluids or tissues of infected fruit bats or primates. Sexual contact can also facilitate transmission, including contact with people who seem to have recovered from the disease, but who are convalescing long-term.
The CDC says that ebola is not usually transmitted by ingestion, although it is believed that, in some areas of the world, it can be transmitted by the handling and skinning of bushmeat via close contact with infected bodily fluids.
Ebola is not known to be transmitted by mosquitoes or ticks.
What is the current status? The current outbreak is on-going in the North Kivu and Ituri provinces of Congo. The most recent report identified 372 confirmed cases and 47 probable cases involving 240 deaths and 123 cures. Fifty-nine suspected cases were listed as under investigation.
Experimental vaccines and treatment have been apparently successfully during the present outbreak. However, since the outbreak is located in an active conflict zone, healthcare providers are faced with a number of other challenges that make fighting the outbreak.
Can livestock be affected by ebola? Scientists believe that pigs are the only species of livestock with the potential to be affected by ebolavirus. However that particular form of infection is not considered a threat to people, and has not been reported outside of a laboratory setting. Dogs eating dead infected animals appear to resist infection and develop antibodies.
What is CEEZAD doing? Dr. Jean-Paul Gonzalez, CEEZAD’s deputy director, is part of a team sponsored by the U.S. government that identifies personnel and methods capable of responding to the present outbreak in the DRC. Dr. Gonzalez and his team identified for the first time chiropterans as a potential carrier of ebolavirus. They also demonstrated the natural circulation of the ebolavirus antigen without outbreak occurrence in Central Africa. During the 2014 outbreak in Sierra Leone, he also took part of the ebola early response team in Sierra Leone.-
- - - - - - - - -
Sources: CEEZAD, Centers for Disease Control, webmd.com, promedmail.org
November pathogen of the month:
Anthrax
What is it?
Anthrax is a serious bacterial infection affecting people who come into contact with bacillus anthracis, generally by way of infected animals or contaminated animal products. Moreover, domestic and wild animals can become infected when they inhale or ingest spores—an environmentally resistant form of the bacteria -- in contaminated soil, plants or water. The CDC says anthrax can be acquired in four ways: by skin-to-skin contact, by inhalation of spores, by eating the spores, or by injection.
Who is at risk? Most people will never be exposed to anthrax. However, Some daily activitiies can pose a greater risk of exposure. Those activities involve people whose careers involve handling animals: veterinarians, livestock producers, and laboratory professionals. Wild fauna – hippopotami, antelopes, zebras and otters -- are regularly exposed, and can redistribute the bacteria. Anthrax can also be passed by contact via the use of products made from dried animal skins such as drums if the raw materials for those items came from an endemic area. During a bioterror event, the risk also exists for mail handlers, military personnel and response workers.
Weaponized Anthrax: Because they can be easily produced in a lab, anthrax spores can be weaponized. The spores can be released quietly and without anyone’s knowledge by their introduction into sprays, food and water.
What is the current status? Last month, outbreaks of anthrax were reported in India and Kenya. In Kenya, the outbreak was reported in a village where it was hoped the damage would be confined to animals. That was not the case in India, where the outbreak began in mid-month. At least seven serious cases of anthrax in humans were reported after the victims came in contact with meat from infected cattle. There, animal husbandry officials undertook a vaccination drive or cattle in a six-mile radius of the affected village on what was described as a “war footing.”
How serious can it be? Bacillus anthracis is designated by the U.S. government as a “Tier 1” agent because it presents “the greatest risk of deliberate misuse with significant potential for mass casualties or devastating effect to the economy, critical infrastructure, or public confidence.” Anthrax is a versatile agent. In 2001 spores were placed in letters and mailed. It can also be released into the air from a truck, building or plane.
Is there a vaccine? A vaccine does exist, but it is currently provided only to people understood to be at an increased risk of coming in contact with anthrax spores. The vaccine is not licensed for children under 18, pregnant or nursing women, or adults over age 65.
Are there effective treatments? Anthrax can be efficiently treated by trained medical personnel with the use of appropriate antibiotics. Once anthrax toxins have been released into the body, antitoxins can also be used with other treatment to counteract the disease’s impact.
- - - - - - -
Sources: www.cdc.gov; www.thehindu.com/newws/cities/Vijayawada/seven-persons-diagnosed-with-anthrax-in-chittoor-district/article25439805; www.promedmail.org; ceezad staff.
October pathogen of the month:
African swine fever
What is it?
African swine fever is a highly contagious hemorrhagic disease of domestic pigs and wild boar. It is characterized by high fever, loss of appetite, hemorrhages in the skin and internal organs, and death in 2-10 days with most isolates. Mortality rates may be as high as 100%.
The organism which causes ASF is a DNA virus of the Asfarviridae family. Due to the high mortality rate and absence of any vaccine, it can have a tremendous economic consequence for the pork production industry. However, humans are not susceptible to ASF.
What is the current status?
The disease has been endemic across sub-Saharan Africa and eastern Europe, and a few months ago found its way eastward into China and westward into Belgium. Those facts concerned those involved in the pork industry due to the fact that China produces nearly half the world’s pork.
Apart from the outbreaks in China and Belgium, ongoing ASF outbreaks have also been reported during September in the following countries: Poland, Hungary, Ukraine, Romania, Moldova, Latvia, Russia and Bulgaria.
How serious can it be?
Due to its potential impact on the world’s food supply, ASF is considered to be a serious economic threat. That threat is intensified by the ease with which ASF appears to spread, apparently being cared by populations of wild boars that obviously have the ability to cross even closely monitored international borders.
What is CEEZAD doing about African swine fever?
The efforts to enhance general knowledge about the ASF threat, to improve diagnostic tools and to develop a vaccine are each major focal points of CEEZAD’s research program.
Dr. Juergen Richt, CEEZAD’s director and an internationally recognized expert on transboundary animal diseases, was in the Far East on a series of presentations when the outbreak occurred in China. Dr. Richt spoke with veterinary medicine faculty and students at Konkuk University in Seoul, and also with members of the media and swine associations in South Korea to update them on the potential threat in their country.
Dr. Richt was Principal Investigator of a CEEZAD-based research project that worked on an ASF vaccine approach based on prime-boost vaccination. In parallel, gene-deleted ASF viruses to be used as modified live virus vaccines have been developed using CRISP-Cas9 knock-out approaches. Both projects were in collaboration with Dr. Yolanda Revilla at Centro de Biologia Molecular Severo Ochoa in Madrid.
CEEZAD also co-sponsored a June presentation on ASF by Dr. Armanda Bastos, a professor of veterinary microbiology and conservation genetics at the Mammal Research Institute of the Department of Zoology and Entomology at the University of Pretoria in South Africa. Dr. Bastos reported on her research into the prevalence of the species of tick that is responsible for the distribution of ASF, in the northern regions of South Africa, notably the Kruger National Park and the Mkuze Reserve. Based on the new research, Dr. Bastos said she believes eradication of the virus is “doable,” but will require intense and ongoing surveillance.
With respect to diagnostics, Dr. Richt leads CEEZAD efforts to develop tests for the detection of nucleic acid markers of ASFV and anti-ASFV antibodies in different samples like oral fluids and meat juice. Work is also being done on point-of-care detection of ASFV using a portable detection device.
Sources: Centers for Disease Control, oie.int, www.ceezad.org, http://www.cvmbs.colostate.edu/aphi/feralswine/PDFs/Rassow_paper.pdf
September pathogen of the month:
Plague
What is it?
Plague is a bacterial disease transmitted by the fleas that infest on rodents. For most of the past century, plague in the United States has chiefly been found in rural and semi-rural areas of the West where many types of rodents can be found.
Many types of animals can be infected by plague. Wild carnivores can be infected by eating other infected animals. Such plagues can become epizootic, infecting humans.
History of plague
Plague has a notorious medical history dating back to ancient times. The first recorded pandemic, the Justinian plague, began in 541 and over the next two centuries was estimated to have killed 25 million people. The Black Death or Great Plague began in China in 1334 and spread through Europe, claiming an estimated 60 percent of the European population. The most recent major spread of plague broke out in China in the 1860s and spread across the world by rats aboard steamships. It causes an estimated 10 million deaths.
What is the current status?
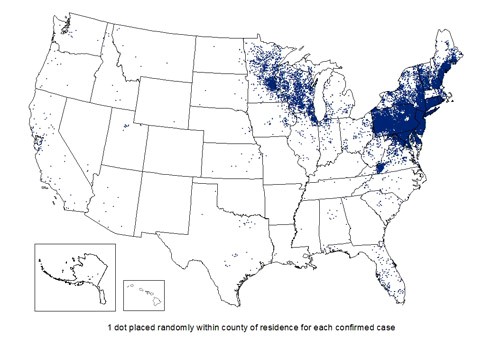
The accompanying map shows the distribution of bubonic plague cases since 1976. A cat in Wyoming was recently confirmed to have been infected with plague. The case comes a little over a year after the plague was found in prairie dogs in the Thunder Basin National Grassland.
The last confirmed case in a human in Wyoming was in 2008, according to a department press release. Overall, there have been just 6 cases of plague in humans in Wyoming since 1978, according to the department. The United States overall averages 7 human cases a year.
"Plague is a serious bacterial infection that can be deadly for pets and for people if not treated as soon as possible with antibiotics," Alexia Harrist, state health officer and epidemiologist, said in a statement. "The disease can be transmitted to humans from ill animals and by fleas coming from infected animals."
Worldwide, Plague epidemics have occurred in Africa, Asia, and South America. Most human cases since the 1990s have occurred in Africa. Almost all of the cases reported in the last 20 years have occurred among people living in small towns and villages or agricultural areas rather than in larger towns and cities.
How serious can it be?
The Centers For Disease Control says Plague is a very serious illness, but is treatable with commonly available antibiotics. The earlier a patient seeks medical care and receives treatment that is appropriate for plague, the better their chances are of a full recovery.
Prevention
The CDC lists several basic steps to minimize one’s risk of being exposed to Plague: These include: Reduce rodent habitat around your home, work place, and recreational areas; wear gloves if you are handling or skinning potentially infected animals to prevent contact between your skin and the plague bacteria; use repellent if you think you could be exposed to rodent fleas during activities such as camping, hiking, or working outdoors; keep fleas off of your pets by applying flea control products. Animals that roam freely are more likely to come in contact with plague infected animals or fleas and could bring them into homes; do not allow dogs or cats that roam free in endemic areas to sleep on your bed.
Source: Centers for Disease Control.
August pathogen of the month:
Norovirus
(The most common cause of gastroenteritis)
What is it?
Norovirus is a highly contagious virus known for its tendency to spread quickly in densely populated areas, as well as through contaminated food. Since it has a reputation for moving freely in areas with large numbers of confined people, it is informally known as a “cruise ship virus,” although it is also common in college dorms and restaurants. However, it is also known to be able to spread quickly via water – in such settings as swimming pools, making it a particular threat in summer. Symptoms include vomiting, diarrhea, and other gastrointestinal symptoms. Norovirus can live in water for several months or possibly even years, the Centers for Disease Control has said -- and lakes and ponds can pose a particular risk, since they're not treated with germ-killing chlorine.
The Centers for Disease control estimates that norovirus causes 19 to 21 million cases of acute gastroenteritis annually, contributing to as many as 71,000 hospitalizations and up to 800 deaths in the United States alone. The case fatality rate worldwide is about 7 persons per 100,000.
What is the current status?
Two recent outbreaks in the United States have thrust norovirus into the news. A July outbreak in Maine sickened nearly 100 people who visited a beach and swam in a lake in the town of Bridgton or had contact with others who had done so. Several people became ill after caring for someone who'd been at that beach and got sick -- even though they hadn't been to the beach themselves. That makes sense, say health officials, since norovirus can also spread through direct contact with infected people.
Also in July, a food court illness that sickened 350 people in Kentucky was identified as norovirus. Citing a Lexington-Fayette County Health Department release, the Lexington Herald-Leader reported that test results from those who had gone to the Fayette Mall food court were consistently positive for the very contagious virus.
How serious can it be?
The illness, which is often characterized as “food poisoning” or “stomach flu,” is not usually serious. There is no treatment, but most people get better within one to 2 days.
Even so, persons with a norovirus illness should drink plenty of liquids to replace fluid lost from vomiting and diarrhea. This will help prevent dehydration, which can lead to serious problems. Severe dehydration may require hospitalization for treatment with fluids given through your vein (intravenous or IV fluids).
Watch for signs of dehydration in children who have norovirus illness. Children who are dehydrated may cry with few or no tears and be unusually sleepy or fussy.
Prevention
The Centers for Disease Control recommends several common-sense steps designed to reduce the risk of being affected by a norovirus. These steps include practicing proper hand-washing, the safe handling and preparation of food, cleaning and disinfecting surfaces and thorough washing of laundry. It also emphasizes that those who are showing symptoms of norovirus should not engage in the preparation of food for others.
Sources: Seattle Pierce County Health Department; oie.int; Lexington Herald-Leader; Centers for Disease Control.
July pathogen of the month:
Rift Valley Fever
What is it?
Rift Valley Fever (RVF) is a disease of humans and ruminant animals (cattle, buffalo, sheep and goats) caused by a virus that is spread through mosquitoes. It is also spread to humans by direct contact with blood, fluids, or tissues of infected animals.
In animals, Rift Valley Fever can cause severe disease, death and abortions, resulting in serious economic consequences. In humans, symptoms include fever, weakness, back pain, dizziness, and weight loss. People usually recover in two days to one week. However, some people may suffer more severe illness, such as severe bleeding, inflammation and swelling of the brain, or eye disorders. About 1-10% of infected people may have permanent loss of vision. Approximately 2% of people who get RVFV die from the infection.
What is the current status?
A recent outbreak of Rift Valley Fever is causing widespread losses and illnesses in Eastern Africa, notably Tanzania, Rwanda, Kenya and South Africa. In parts of Kenya, where the disease was first identified in 1931, slaughterhouses have been closed for weeks following a recent outbreak. There, 26 human cases have been reported, six of them fatal. A regional meeting of a council on Agriculture and Food Security in Dar es Salaam, Tanzania directed East African nations to address the issue of Rift Valley Fever promptly.
How serious can it be?
2016 outbreaks in Uganda and Niger identified nearly 350 human cases, 33 of them fatal. In ruminants, losses translate to animals that do not enter into the food chain, and to an increase in abortions resulting in decreases of future generations of animals. Impacts are also measure in decreases to the availability of dairy products. The Centers for Disease control says analysts characterize the potential disruption to the economy of a stricken nation as devastating.
Prevention
The best prevention steps involve control of the mosquito vector as well as vaccination campaigns.
What’s CEEZAD doing about it?
CEEZAD scientists Juergen Richt, Igor Morozov, and Bonto Fabuary, working in conjunction with USDA research microbiologist Bill Wilson, are engaged in the development of a safe, efficacious and DIVA-compatible vaccine to prevent ruminant animals from developing Rift Valley Fever.
Sources: CDC, CEEZAD.org, World Health Organization, Promedmail.org
June Pathogen of the Month:
Lyme Disease
What is it?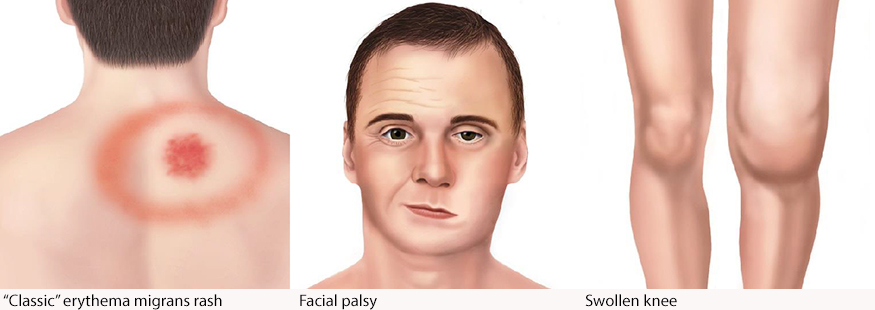
Lyme disease is a chronic, debilitating disease. It could be caused by the bacterium Borrelia burgdorferi and transmitted to humans by the bite of infected blacklegged ticks,although scientists believe its worldwide nature make it possible that other bacterium and/or other vectors could also be involved. That possibility is under study. The riskiest months for Lyme Disease are typically May through September when young ticks are biting. Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans.
What is the current status?
The disease, which is widespread in the northeast and Great Lakes areas, has recently been reported to be spreading in Canada. Although concentrations are heavier in the northeast and Great Lakes areas, Lyme Disease is widespread in the United States during summer months. In 2016, there were more than 36,000 confirmed or suspected cases in all but three states, including 16 confirmed and 23 suspected cases in Kansas. Worldwide, the Lyme Disease Association has identified Lyme Disease in more than 80 countries on every continent except Antarctica (see map).

How serious can it be?
Lyme Disease is a serious, acute and chronic, multi-systemic disease that can have long-term consequences for those affected by it. It can attack many tissues, including the heart, colon and nervous system. Even in cases where treatment is successful in relieving symptoms, it is not unusual for that two-to-four week treatment period to be followed by lingering symptoms of fatigue, joint pain or muscle aches, sometimes lasting several months.
Prevention
The Lyme Disease Association emphasizes use of tick repellents, proper clothing, tick checks and proper tick removal techniques after outdoor activities as the most effective prevention steps.
Sources: CDC, CEEZAD.org, Lyme Disease Association Inc.
May Pathogen of the Month:
Ebola
What is it? 
The World Health Organization describes Ebola as a severe, often fatal viral disease. Ebola first appeared in 1976 in Africa near the Ebola River, giving the illness its name. Symptoms include the sudden onset of fever fatigue, muscle pain, headache and sore throat. The disease can be difficult to distinguish from other infectious viruses. The virus has also shown some ability to persist and therefore be passed along by patients who have recently recovered from its effects.
What causes its spread?
Ebola is transmitted to humans from wild animals, the most likely source being the fruit bat. Those bats are believed to be the source of infection, transmitting the virus to chimpanzees, gorillas, monkeys, forest antelopes and porcupines, who in turn pass it to humans through close contact with blood, organs, secretions or other bodily fluids. But it can also be spread via human-to-human transmission by direct contact and eventually by sexual contact.
How widespread is it?
The most recent serious outbreak was in 2014-16 in West Africa, its range extending from Guinea to Sierra Leone and Liberia. More than 28,000 cases were reported in those three nations alone with an estimated 11,310 fatalities.
What is CEEZAD doing about it?
The December 2017 edition of Medecine et Sante Tropicale includes an article co-written by Dr. Jean Paul Gonzalez, CEEZAD’s deputy director, on recent developments in the effort to contain Ebola.
Sources: WHO, CEEZAD.org, epainassist.com, NewsnViews.
April Pathogen of the Month:
Leishmaniasis
What is it? 
The World Health organization describes leishmaniasis as a disease caused by the protozoan Leishmania parasites transmitted by the bite of infected female phlebotomine sandflies. There are three main forms of leishmaniases – visceral (also known as kala-azar and the most severe form of the disease), cutaneous and mucocutaneous, the most common. The disease affects some of the poorest people on earth, and is associated with malnutrition, population displacement, poor housing, a weak immune system and lack of financial resources.
What causes its spread?
Leishmaniasis is linked to environmental changes that disturb the ecosystem of the sandfly vectors such as deforestation, building of dams, irrigation schemes, and urbanization.
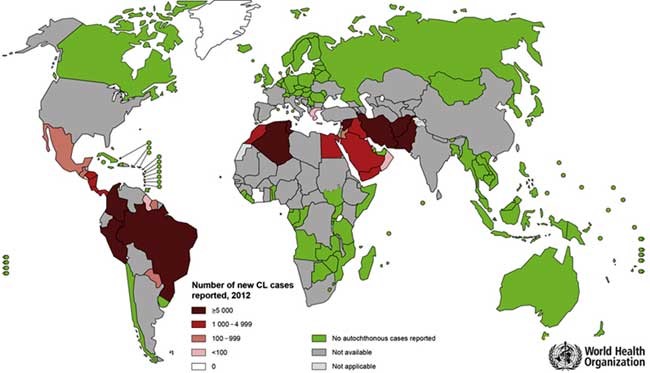
How widespread is it?
The WHO estimates that 700,000 to 1 million new cases occur annually, with between 20,000 and 30,000 deaths worldwide.
Have outbreaks occurred recently?
Yes. In March, a medical organization documented about 35,000 cases of infection with leishmaniasis in northern and central Syria. Last year, about 70 cases of visceral leishmaniasis, also known as the black fever, were diagnosed in Syria.
What is CEEZAD doing about it?
The March 2018 edition of the American Journal of Tropical Medical Hygiene included an article co-written by Dr. Jean Paul Gonzalez, CEEZAD’s deputy director, on the causes of leishmaniasis infection in Libya. In the paper’s abstract, the article’s authors report on findings from their screening of sandflies for leishmanial DNA.
Sources: OIE, WHO, CMAJ, Pasteur Institute, Libyan National Center For Disease Control, University of Sabratha, University of Tripoli.
March Pathogen of the Month:
Hantavirus
What is it?
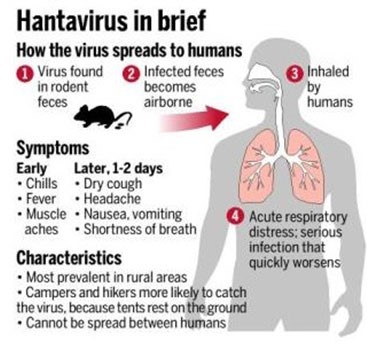
Hantavirus Pulmonary Syndrome, known more simply as hantavirus, is a severe and potentially fatal respiratory disease in humans. It is carried by rodents, making it a potential threat even to those living in homes. Human-to-human transmission has not yet been reported in the United States, although rare cases of human-to-human transmission have been reported elsewhere.
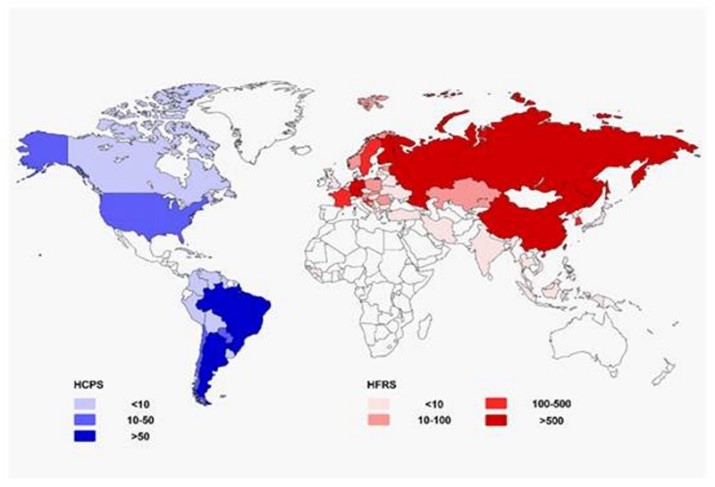
Where is hantavirus
The Centers For Disease Control has been monitoring hantavirus infections since 1993; to date, more than 700 cases have been reported, 16 of them in Kansas. The virus appears to be more widespread in South America, with individual and small clusters of cases reported in nine nations on that continent. Large outbreaks are rare, but they can be serious. Scientists have listed the mortality rate from hantavirus at 38 per cent. Last year an outbreak in Washington state claimed three lives. Hantavirus extends worldwide and shows different clinical presentations and severities (see map). These presentations include HCPS and HFRS.It is most commonly found in rural areas with abundant forests, fields and farms for the rodent host.
Symptoms
Humans are most at risk when they engage in activities with the potential to put them in contact with rodent urine, droppings, saliva or nesting materials. This can include sweeping and dusting. Opening or cleaning cabins, outbuildings and other structures closed for the winter can also present concerns. Campers and hikers can also be exposed. Hantavirus symptoms include fatigue, fever and muscle pains, particularly in the large muscle groups. These can be accompanied by headaches, dizziness, chills and abdominal pain, nausea, vomiting, and diarrhea.
Are there current outbreaks?
Yes. In January and February the nation of Chile reported five cases of hantavirus infection, one of them fatal. In February, an Arizona woman contracted a disease subsequently diagnosed as hantavirus. Cases have also recently been reported in New Mexico and Colorado.A 2017 outbreak of Seoul virus infection, a version of hantavirus, was identified in 31 infected ratteries in 11 states, among them Iowa and Colorado. Seventeen human infections were reported.
Sources: CEEZAD; Centers for Disease Control; Reuters
February Pathogen of the Month:
Crimean Congo Hemorrhagic Fever
What is it?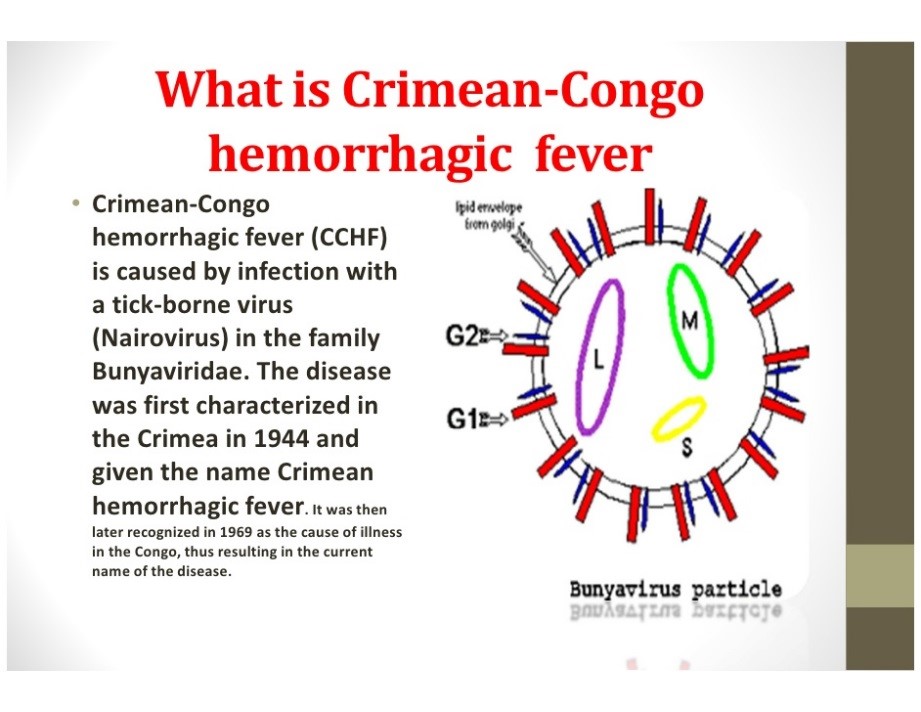
Crimean Congo hemorrhagic fever is a disease that causes severe bleeding in humans and animals. The virus, which is carried by ticks, kills 10 to 40 percent of its victims. It can also be transmitted to people through direct contact with infected animal blood or tissues. Human-to-human transmission is possible due to close contact with secretions from infected persons. Symptoms include fever, muscle ache, dizziness, neck pain, headache and light sensitivity. Nausea, vomiting and diarrhea also occur.

Where is Crimean Congo hemorrhagic fever?
CCHF is endemic in Africa, the Balkans, the Middle East, and various Asian countries south ofthe 50th parallel north -- the present geographical limit of the principal tick vector. It has not yet established an ongoing presence in Western Europe, although researchers believe that could happen absent effective control strategies. The hosts of the CCHF virus include a wide range of wild and domestic animals such as cattle, sheep, and goats. For this reason, animal herders, hunters, livestock workers and slaughterhouse workers are viewed as being particularly at risk.
Is it a threat to humans?
Very much so. In January of 2018, an outbreak of what is known in Africa as 'Bleeding Eye Fever' killed four and infected dozens in South Sudan, Uganda and other areas of east Africa. In South Sudan, health chiefs warned that the spread could be "catastrophic". Up to 60 people were suspected to be infected, and were undergoing tests by a team from the Sudanese health ministry and the World Health Organization. It is difficult to prevent or control CCHF infection in animals as the tick-animal-tick cycle usually goes unnoticed and the infection in domestic animals is usually not apparent. Furthermore, the tick vectors are numerous and widespread, so tick control with chemicals is only a realistic option for well-managed livestock production facilities. In a possible response to climate change, tick vectors also appear to be moving westward from their historical distributions toward wetter environments.
What is CEEZAD doing about Crimean Congo hemorrhagic fever?
CEEZAD scientists have partnered with and support the research of Dr. Huseyin Yilmaz, a veterinarian at Istanbul Veterinary School in Turkey, whose work includes research into the epidemiology of CCHF.
Sources: World Health Organization, Centers For Disease Control, slideshare.net.
January Pathogen of the Month:
Avian Influenza
What is it?
Avian influenza is the infection of birds with the Type A strain of the influenza virus. This virus is endemic worldwide, and can infect both domestic and wild avian species. Avian influenza A is very contagious among birds via nasal, salivary or fecal secretions. With particular respect to domestic birds, avian influenza is a concern for several reasons. The most significant is the potential economic impact on the food animal chain. A second reason is the potential for trade restrictions put into place out of concern for such economic impact. The third reason is the possibility that avian influenza A viruses could be transmitted to humans.
Where is avian influenza
Outbreaks of avian influenza have been reported worldwide. In December of 2017 alone, there were significant outbreaks in China, South Korea, Taiwan, Cambodia and Netherlands.
Its economic impact
The Food and Agriculture Organization estimates that since 2003, global losses from avian influenza outbreaks have run into the billions of dollars. That economic impact depends on the speed with which it is controlled, the extent of its spread, the role played by poultry in the GDP of the affected nation, and the structure of the poultry sector. A 2003 outbreak resulted in the deaths of 44 million birds in Vietnam and 29 million in Thailand, respectively 17.5 and 14.5 percent of those nations’ bird populations.
In the United States, a 2014-15 outbreak of avian influenza affected a reported 49.7 million birds from 211 commercial flocks and 21 backyard flocks, mostly but not entirely in Minnesota and Iowa. That outbreak caused an 11 percent reduction in the egg supply, increasing the cost of a dozen eggs from $1.36 in January to $2.06 in July.
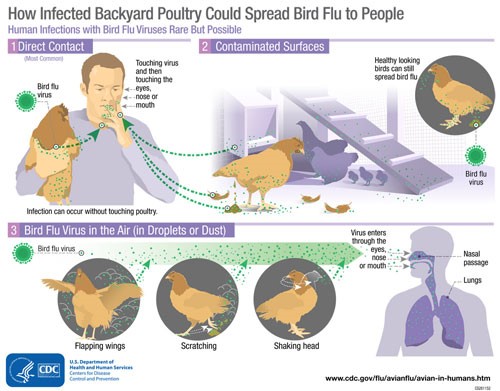
Threat to humans
The CDC considers the risk of avian influenza to human health to be low at present. It recommends, however, that people should observe wild birds only from a distance, avoid contact with domestic birds that appear ill or that have died, and avoid contact with surfaces that appear to be contaminated with fecal matter from wild or domestic birds.
What is CEEZAD doing about avian influenza?
Researchers supported by CEEZAD have developed live and inactivated Newcastle Disease virus-vectored vaccine candidates protecting chickens against the avian influenza virus. The vaccines were shown to be protective against novel H5NX strains for the recent outbreak in the U.S.
Sources: CEEZAD; Centers for Disease Control; Applied Commodity Price Analysis, Forecasting and Market Risk Management; Food and Agriculture Organization.